Case Studies
Analyzed symptoms are chosen by the effect they have on quality of life of a particular patient...

29 Jan 2020
About Multiple Sclerosis
Basic Features of the Progressive Form of MS
Disease-Modifying Drugs in the Treatment of PPMS
Rehabilitation Strategies
Nutritional Support
Stem Cells as a Promising Approach to Manage PPMS
MSCs-Based Treatment Procedure
MSCs Collection
Procession and Cultivation of Harvested Cells
Bioactivation of MSCs
Administration of Cell Products
Supplemental Procedures
List of References
About 2.2 million people globally suffer from multiple sclerosis (MS), which makes this disease the most common disorder of the central nervous system [1]. This chronic condition affects mostly young adults in their 20s–40s. During the course of the disease, focal lesions are formed in the brain and spinal cord. They consist of neuronal cells that have been damaged by the person’s own immune system. The process of neuronal damage is called demyelination because the immune system destroys myelin, which is the protective substance that covers neurons. Demyelination is also accompanied by inflammation in the damaged area, as well as damage to the neuronal fibers.
In the majority of patients, multiple sclerosis starts with a relapsing-remitting course (RRMS), which may at later times transform into the secondary progressive form of the disease (SPMS).
In some 10–15% of patients, progression is observed from the very beginning of the disease without an initial relapsing-remitting phase [2]. This subtype of MS is called primary progressive multiple sclerosis (PPMS) which, on average, starts later in life than the relapsing-remitting subtype, typically starting in a patient’s 40s–50s.
Neuron damage caused by the immune system’s activity leads to impairment of various functions, primarily motor activity and balance due to lesions in PPMS being mainly localized in the spinal cord. Common symptoms in patients with this type of MS include:
This video demonstrates the changes to normal neuron functions in MS patients and the mechanism of symptom occurrence:
The mechanism of action of the currently approved disease-modifying drugs is realized through reducing inflammation in the central nervous system which slow-downs the disease progression, prolongs the period of remissions and stabilizes some symptoms. However, these drugs show little efficacy in PPMS since this subtype is characterized by greater nerve degeneration and a lesser level of inflammation than in other types of MS.
The sole drug that has demonstrated a reasonable level of efficacy in PPMS patients is ocrelizumab. It inhibits the immune system by binding and killing certain types of white blood cells that are responsible for demyelination [3].
Ocrelizumab was approved by the FDA on the stipulation that the manufacture will conduct additional post-marketing clinical trials to clarify its safety profile [4]. The following serious side effects of ocrelizumab were registered during clinical studies and needs further investigation:
Like other immunosuppressive drugs, ocrelizumab may cause other common adverse reactions like infections, fever, fatigue, nausea, skin reactions, flushing, throat and mouth irritation, and rapid heart rate.
Some trials in which ocrelizumab was studied in other autoimmune diseases (rheumatoid arthritis and lupus) were discontinued due to an extremely high rate of serious infections [5].
Besides basic treatment with ocrelizumab, additional therapy to control symptoms may be required. It includes both specific medications and physical therapy. Physical activity itself can help decrease inflammation by modulating the immune system [6, 7, 8, 9, 10].
Regular exercise can increase muscle strength needed to deal with balance and coordination issues, increase the health of the heart, mitigate fatigue and spasticity, improve the emotional status and stabilize mood.
A comprehensive multidisciplinary rehabilitation has been shown to ease the burden of MS symptoms by improving self-performance and independence. It includes physiotherapy, stretching and positioning techniques, and gait and balance training, among others [11].

Figure 1. Physical activity and exercise play a pivotal role in symptom management and help to regulate immune system activity.
There are some indications that diets and nutritional habits may support treatment and help to reduce the signs and symptoms of MS.
It was shown that vitamin D, apart from its role in calcium metabolism and bone formation, modulates the immune system and regulates cell growth and, therefore, reduces MS disease activity. The best sources of vitamin D are fatty fish, milk and milk products, fortified fruit juices, beef liver, cheese, egg yolks, and cereals.
Biotin, a form of vitamin B, was studied in people with primary-progressive MS or secondary-progressive MS. In some patients, biotin in high doses was able to improve disability without serious safety issues. Biotin is contained in meat, eggs, nuts, seeds and some vegetables such as broccoli, cauliflower, sweet potatoes, and spinach. It is also widely available in a supplement form.
Food rich with Omega-3 (fatty fish, cod-liver oil, or flaxseed oil) and Omega-6 (sunflower or safflower seed oil, possibly evening primrose oil) and a diet low in saturated fats may have some benefit for people with MS.
Other products that are considered to be helpful for patients with MS are:
Stem cells have become the focus of intense research for the latest decades in the context of the treatment of various diseases. Using mesenchymal stromal cells (MSCs) derived including from bone marrow, contains potentially beneficial properties that can repair and protect cells of the central nervous system and, therefore, can modify the course of PPMS.
Normally, several bone marrow cell subpopulations participate in spontaneous tissue repair [13, 14, 15]. The MSCs are the most studied type of bone marrow cells, displaying pronounced immunomodulating and immunosuppressive properties, promoting myelin repair and also possessing other reparative effects [16, 17, 18, 19]. They demonstrate both powerful neuroprotective properties and anti-inflammatory activity and provide trophic support for the injured areas of the nervous system [20, 21, 22, 23, 24, 25].
MSCs can fuse with specific cell types, in particular, damaged tissue cells, apparently representing a further mechanism by which MSCs may offer protection for damaged cells [21, 25].
The effects of MSCs are realized through the vast range of bioactive factors they produce (cytokines, chemokines, growth factors, etc.).
According to some studies, both endogenous MSCs, which naturally exist in the patient’s body, and administered MSCs in a certain amount are able to migrate to the spinal cord and precisely target damaged tissue [26, 27, 28, 13].
MSCs reside not only in bone marrow but also in other adult tissues (such as adipose tissue, placenta, umbilical cord, and several others) which can be used as sources for therapeutic cells, as well [29, 30]. Due to their simple isolation procedure, as well as their potential to migrate to damaged areas, MSCs are ideal candidates for different cell therapies.
The efficacy and safety of stem cells derived from bone marrow have also been shown in an increasing panel of studies [31, 32].
Though the ability of stem cells to assist in the treatment of certain diseases has been proven, they cannot be considered as a guaranteed cure for all patients. The effectiveness of the therapy depends on multiple factors: diagnosis, initial condition, stage of the illness, severity of symptoms, age of the patient, hereditary predisposition, lifestyle, etc.
Find out if stem cell therapy is beneficial for you >>>

Figure 2. Patient’s stem cells procession and activation prior to being introduced back into the patient’s body.
MSCs-based treatment is a rather simple and painless procedure. It usually includes 4 steps:
The usual source of MSCs is the patient’s bone marrow, adipose tissue or donated tissues, such as the placenta or umbilical cord (Wharton’s jelly). Thus, cells may be both donated and autologous (patient’s own). The process of obtaining cells is performed under local anesthesia.
Harvested MSCs undergo centrifugation and then are cultivated in special media to obtain pure cell products with sufficient quantity and quality of cells.
Bioactivation allows an increase in the beneficial features of the cell product.
The prepared cell product may be introduced locally, intrathecally into the spinal canal and/or intravenously through an IV drip, depending on the treatment plan.
When cell-based products prepared from donated tissues are used, they can be introduced immediately because they are prepared priorly. The use of donor stem cells also lets the patient avoid the extraction procedure, which is beneficial if the anesthesia for the patient is contraindicated for some reason.
The MSCs-based treatment is most effective if combined with physiotherapy. The treatment plan is customized depending on the duration of the patient’s symptoms, stage of disease progression and other factors. The following procedures are advised for all patients with MS, including PPMS, in addition to basic treatment with MSCs:
along with some others.
Only using stem cells to treat multiple sclerosis may not be enough in most cases. Cell-based therapy works more effectively when combined with some of these therapeutic methods which help activate the tissue repair process.
Contact Medical Advisor to learn more about the results you can expect from stem cell therapy >>>
– Published on January 29, 2020
Testimonials
What they say about us
Shaun Lawrence battled multiple sclerosis for many years before deciding to come to Swiss Medica clinic. Limp on his right leg, urinary and bowel problems were some of the main issues he suffered from. After having a stem cell treatment his life changed completely. He is very satisfied with the experience, as well as the overall results of the treatment.
continue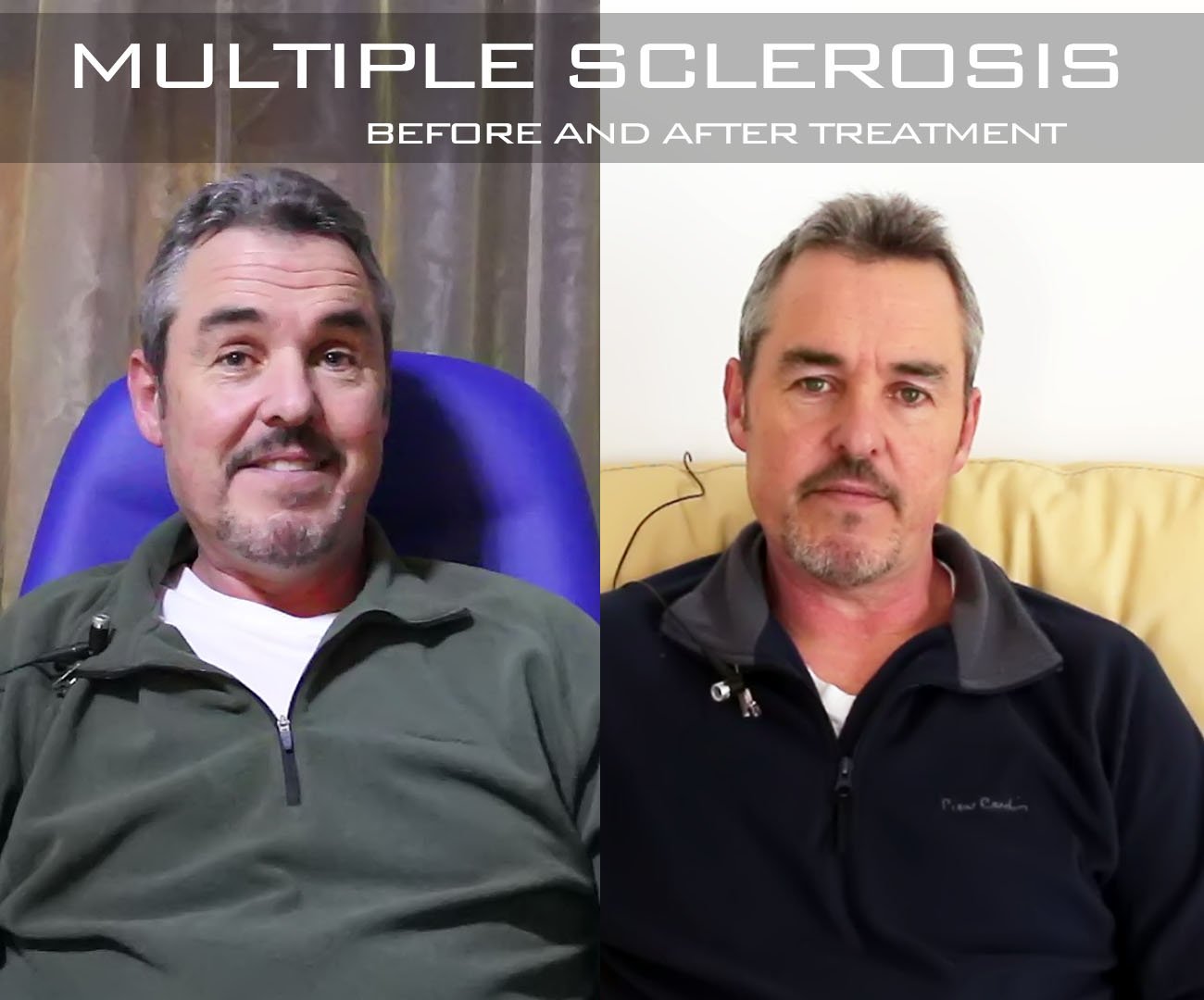
For me, since I got back after my 2 weeks of having my treatment, within 2 days of being home speaking to friends and family around the world, they all noticed the difference in my speaking, cognitively and I was able to listen and integrate with conversations with my family at home.
A wonderful experience, a wonderful care are these very caring people, yes.
continue
Everything is done naturally and pleasantly here. Actually I do not feel sick, it is the most important thing – during these 12 days I haven’t felt sick.
I didn’t have the impression that I was treated like a patient. I was treated like a normal person, it is true I take medicines, receive infusions and still have some pain, but I never felt like I was in the hospital.
continue
Linda Cole struggled with multiple sclerosis for over 30 years. She decided to give stem cell treatment a try, even though she didn’t expect much from it. She was pleasantly surprised, as her symptoms improved and reversed drastically. Her ability to move, walk and think much better than before assured her she made the right decision by coming to Swiss Medica.
continueAll form fields are required.